Element 5: Physical and psychological health
5.1 NOISE Page No. 4-13
5.2 VIBRATION Page No. 13-17
5.3 RADIATION Page No. 18-23
5.4 MENTAL ILL-HEALTH Page No. 24-31
5.5 VIOLENCE AT WORK Page No. 31-34
5.6 SUBSTANCE ABUSE AT WORK Page No. 35-37
NOISE
Scope of Learning
The physical and psychological effects of exposure to noise
The most common physical effects from Noise are as follows-
Psychological effects include-

Glossary of Terms
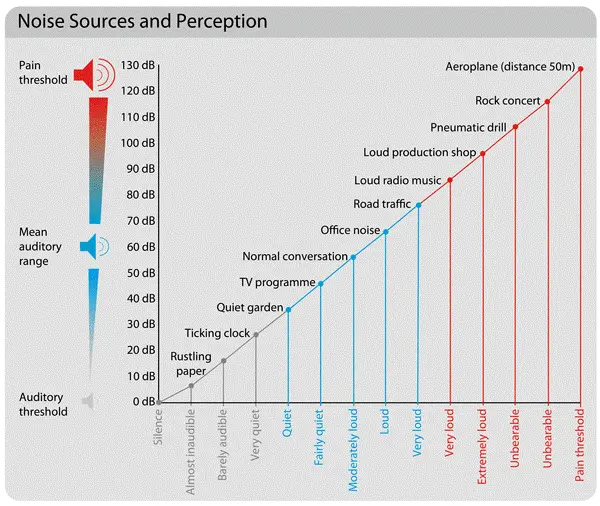
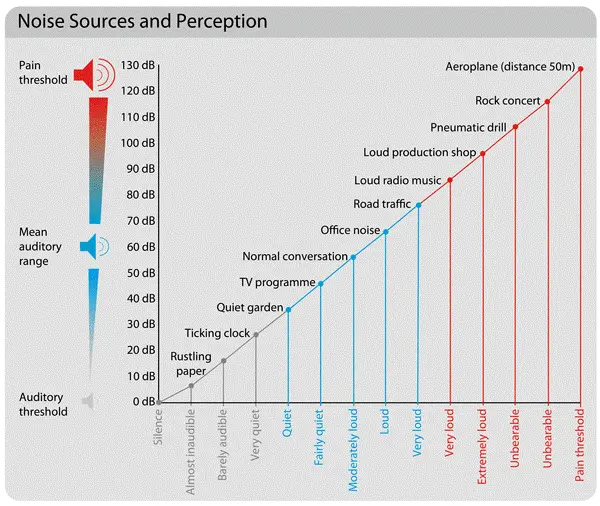
Sound Pressure Level- The instantaneous acoustic pressure is the sound pressure level (Lp or SPL), which is measured in decibels (dB). Since the ear is more sensitive to changes in pressure than to the power or intensity of the source, measuring this parameter shows how it affects people.
Frequency- Frequency is the number of times something happens in one second. It is measured in Hertz (Hz). For sounds, this is what people call pitch.
Decibel- It is estimated that 2 x 105 Pascals (Pa) to 200Pa is the audible sound pressure range. The range is simplified to zero decibels (dB) to one hundred forty decibels (dB) when expressed in dB notation.
A-Weighting– The human ear doesn’t react the same way to all frequencies. Most of the time, A-weighting is used to imitate how the ear responds to different frequencies. It is used to figure out how likely it is that noise will damage your hearing. It is usually written with a capital A in the unit abbreviation (e.g., LAmax, LAeq, etc.) or in brackets after a dB level (e.g., 3dB(A)).
C-Weighting– A common filter that changes the levels of a frequency spectrum in the same way that the human ear does when it hears loud or sudden noises. Most of the time, this weighting is used to judge how something sounds.
Noise Dose– A worker’s total average time-weighted exposure to noise over an 8-hour work day. This is shown as a percentage of the total amount of noise that can be heard. A noise dosimeter can be used to measure noise dose if the worker is exposed to different noise levels at different times of the day. Without a dosimeter, it can be hard to figure out the overall noise dose for different noise levels because you can’t just average the decibel levels. (A logarithmic scale is used to measure noise levels.) Not everyone agrees on the amount of noise that is safe.
Noise Exposure Levels
Why measure Noise at the Workplace?
The most important part of a program to protect workers’ hearing and reduce noise at work is measuring noise levels and workers’ exposure to noise. It helps find places of work with noise problems, employees who may be exposed to noise levels that can cause hearing loss, and places where more noise measurements need to be done. This information also helps figure out what kind of noise-control measures need to be taken.
How is workplace Noise measured?
The sound pressure level is measured to figure out noise exposures for the sake of occupational hygiene. There are many tools and methods that can be used. Which one you choose depends on how loud your workplace is and what information you need. But the first thing to do is figure out if there is a noise problem at work.
How do you identify noise problems in the workplace?
The first step is to figure out if noise could be a problem at your workplace or not. It’s best to do a walk-through survey. Some signs of a potentially dangerous noise level are:
Noise measurement results from research conducted in comparable circumstances are quite useful for identifying the potential noise problem.
What things do you consider when planning noise measurement?
When taking measurements in the field, it is essential to define the type of information needed. The individual making the measurement must comprehend:
The initial measurements are noise surveys to determine if:
The second step is to figure out each employee’s personal noise exposure level, or how much noise they are exposed to. If the noise level at work stays the same throughout the shift and the measurements are representative of a typical day, the data from the noise survey can be used to figure out if there is a risk of exposure to harmful noise levels and if more measurements are needed. But noise dosimetry, like personal noise exposure measurements, is needed if the noise level in the workplace changes during the day or if the workers move around a lot.
What types of instruments are used for measuring noise?
Most of the time, a sound level metre (SLM), an integrating sound level metre (ISLM), or a noise dosimeter is used to measure noise. It’s important to know how to calibrate, use, and read the instrument you are using. Most of this information is in the user’s manual that comes with the instrument.
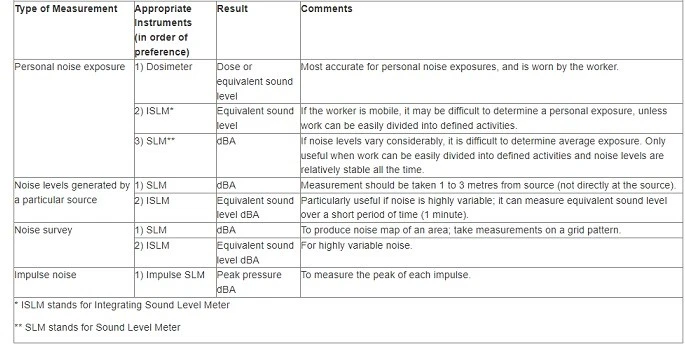
What is a noise dosimeter?
A noise dosimeter is a small, light device that the worker wears with the microphone close to their ear, just above the edge of their shoulder. The noise level information is stored in the dosimeter, which also does an averaging process. It is useful in industries where noise changes in length and volume and where people move around a lot.
A noise dosimeter requires the following settings:
(a) Level of Criteria: 8 hours a day, five days a week is the most time you can be exposed to it. In many places, the criterion level is 85 dBA, but it is 90 dBA in Quebec and 87 dBA in federal Canadian places. The OSH Answers document has more information about the levels of exposure. Limits for noise exposure at work in Canada.
(b) The noise regulation says that the exchange rate is 3 dB or 5 dB..
(c) Threshold: The lowest level of noise at which the dosimeter stops collecting noise dose data.
When a person wears the dosimeter for a full work shift, the average amount of noise exposure, or noise dose, for that person is calculated. Most of the time, this is shown as a noise exposure level, Lex,T. This is a logarithm that takes into account both how much time was actually worked and how much time was exposed. In the past, it was usually given as a percentage of the most it could be exposed to. If a person gets a noise dose of 100% over the course of a work shift, this means that the average amount of noise exposure is the most that can be allowed. For example, if the criterion level is 90 dBA and the exchange rate is 3 dBA, then being exposed to 90 dBA for eight hours gives a 100% dose. A noise dose of 100% is also 93 dBA for four hours. However, 93 dBA for eight hours is a noise dose of 200%.
Noise Action Levels
The Control of Noise at Work Regulations 2005 (Noise Regulations 2005) say that employers must prevent or reduce health and safety risks caused by noise at work. The Regulations also say that employees have to do things.
Under the Noise Regulations, you have to do certain things at certain action levels. These are about:
How much noise your employees are exposed to on average during a work day or week, and how much noise they are exposed to at their loudest (peak sound pressure) during a work day.
The values are:
Lower exposure action values:
Upper exposure action values:
The rest of the employers’ websites will tell you what you need to do. Figure 1’s flow chart will also help you figure out what you need to do.
There are also limits to how much noise someone can be around. These are called exposure limit values:
140 dB peak sound pressure (C)
Noise Control Measures
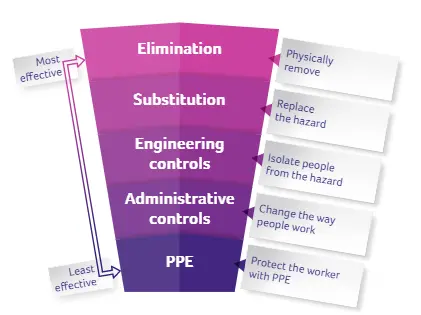
Once the risk of noise has been assessed, the next step is to control the risks.
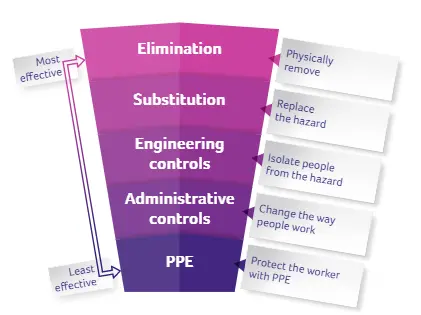
Based on the noise levels found in the noise survey, the hierarchy of control is used to find practical and effective ways to control risks at work. Elimination or replacement of noise sources, group noise control through engineering and work organisation, and personal protective equipment make up the hierarchy of noise control (PPE).
There are many ways to keep noise down, and these will vary from workplace to workplace. There is no one method or solution that works in every circumstance. To figure out the best way to get rid of, reduce, or control the noise, you need to know a lot about what it is, where it comes from, how the plant works, what the workers do, and when they do it.
Factors the organization should consider include:
An important result of a noise risk assessment is finding ways to control the risks and putting them in order of importance. Managers should use the results of the risk assessment to make a formal plan for getting rid of noise. Among the most important steps:
Elimination
Elimination is the best way to keep workers from getting hurt because it gets rid of the noise where it comes from. This isn’t always possible, but some ways to do it would be to stop hard objects or surfaces from hitting each other or to move noisy work away from other tasks.
To cut down on nose at work, it’s important to plan and implement a good buying or renting policy. The most cost-effective and long-term way for a business to lower noise levels is to think early on about how a new work process or piece of equipment would work without making the workers too loud. Before buying new machinery, you should think about how loud it is. You can do this by talking to the manufacturer or supplier of the plant or machinery and getting information from them. This could include how to set up the machine, how to take care of it, and how loud it is likely to be in the conditions where it will be used. Note: Noise levels should always be taken into account when introducing a new work process, choosing new work equipment, or arranging the workstations.
Substitution
Substitution is the process of replacing loud machines or tools with ones that aren’t as loud. When it’s not possible to get rid of the noise-making machinery or equipment, replacing it with quieter ones may be the next best thing to do.
Organizations should always think of different tools and ways of doing work that would make the job less noisy.
Changing the way a job is done can protect the workers by making less noise. For example, using hydraulics to bend materials makes less noise than hammering.
When welding is used instead of riveting, for example, a risk assessment must be done to make sure that it doesn’t introduce a new type of risk.
Engineering controls
Engineering controls are all about making changes to processes, machines, or equipment so that workers are exposed to less noise. For example, workers can be less exposed to noise by using screens, barriers, enclosures, and materials that absorb sound.
Some engineering measures that may be considered are:
Putting more space between the noise source and the factory floor can help.
Administrative controls
Organizing tasks in such a way that fewer workers are exposed to noise for longer periods of time is an example of an administrative control. When eliminating, relocating, or retrofitting sources of noise is not an option, administrative controls should be implemented to decrease exposure levels.
Some administration controls include:
Personal protective equipment
The European Union (EU) uses a single number rating (SNR) for hearing protection, while the United States uses a noise reduction rating (NNR). As a measure of the noise reduction experienced by the wearer, this value in decibels is provided. The average person using an earmuff will experience a reduction in sound pressure of 22–33 dB, while the average person using foam earplugs will experience a reduction of 20–30 dB.
In some situations, the SNR levels won’t be high enough to keep the noise down to a manageable level. As such, new forms of management should be looked upon to reduce workers’ exposure. Workers who are always on the go, like maintenance staff, may find this challenging. Contact industry-specific specialised consultants or organisations for more help on protecting these people, since they will have a wealth of knowledge on how to regulate and manage exposure in the relevant settings.
Correct use of hearing protection is essential for its effectiveness. To ensure the success of HPE training, it is important to test employees’ comprehension of the material thereafter.
Health surveillance
What is health surveillance?
Health surveillance for hearing damage usually means:
Providing health surveillance
You must do health checks (hearing tests) on all of your employees who are likely to be exposed above the upper exposure action values on a regular basis or who are at risk for any reason, like if they already have hearing loss or are more likely to get hurt.
The purpose of health surveillance is to:
References
https://www.hear-it.org/temporary-threshold-shift
https://en.wikipedia.org/wiki/Health_effects_from_noise
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1637786/pdf/envhper00310-0128.pdf https://www.transport.gov.scot/media/6954/app-a8_1-noise-and-vibration-terminology.pdf
http://www.larsondavis.com/learn/sound-vibe-basics/sound-measurement-terminology
https://kb.q-windows.com/benefit/soundproof-aluminum-windows-doors
https://www.ccohs.ca/oshanswers/phys_agents/noise_measurement.html
https://www.hse.gov.uk/noise/employers.htm
https://www.hse.gov.uk/noise/healthsurveillance.htm#what
5.2 VIBRATION
The effects on the body of exposure to hand–arm vibration and whole-body vibration
Mechanical vibrations at work can expose workers to hand-arm vibration (HAV) and/or whole-body vibration (WBV).
Hand Arm Vibration (HAV)- HAV is caused by using tools and doing tasks at work that send vibrations into the hands and arms of workers. It can be caused by hand-held power tools like hammer drills, sanders, grinders, and concrete breakers; hand-guided equipment like powered lawnmowers, chainsaws, and hedge trimmers; or by holding materials being worked on by machines like bench-mounted grinders, pedestal grinders, etc.
Hand-arm vibration syndrome (HAVS) is a group of health problems that can be caused by long-term, regular exposure to HAV. Some of these problems, like vibration white finger and carpal tunnel syndrome, can be permanent and painful..
HAVS affects the hand, wrist, and arm’s nerves, blood vessels, muscles, and joints. If you don’t take care of it, it can make you very sick. Carpal tunnel syndrome is a disorder of the nerves in the wrist that can cause pain, tingling, numbness, and weakness in the hand and wrist. It can happen on its own, but vibration is one of the things that can cause it. Early signs of a problem include tingling and numbness, not being able to feel things with your fingers, losing strength in your hands, and having white fingers that turn red and hurt when they get cold and wet.
Vibration white finger is very painful and can make it hard to move. If vibration continues, it can spread and affect more fingers. Workers who are pregnant, have diseases of the hands, arms, wrists, or shoulders, or have diseases that affect blood flow, like diabetes, are more likely to be affected by HAV. The general and heavy engineering, construction and civil engineering, forestry, and horticulture industries are all connected to HAV.
Whole Body Vibration (WBV)- WBV is caused by machines and vehicles at work that send vibrations up through the seat or down through the feet. It can be caused by driving off-road vehicles, like tractors, over rough surfaces. It can also be caused by excavators digging into hard ground, or by standing close to powerful machines that aren’t moving.
Low back pain has been linked to long-term exposure to high levels of WBV. People who are more likely to be sensitive to WBV include workers who are pregnant, people with neck or back problems, young people whose bones and muscles are not fully developed, and people who have just had surgery. Mining, building, and farming are all industries that work with WBV.
The amount of vibration a person is exposed to is measured by how fast the surface they are in contact with is moving. Most of the time, the speed of the surface is measured in metres per second squared (m/s2).
An accelerometer is a device that is attached to the surface that is moving and gives an output that is proportional to the acceleration. After the frequency weighting has been used, the average size of the vibration is shown.
Typical vibration magnitudes for equipment used at work are as follows.
For HAV:
Chainsaw: 6 m/s2
Sander: 8 m/s2
Hammer drill: 9 m/s2
Road breaker: 12 m/s2
For WBV:
Car: 0.4 m/s2
Lorry: 0.7 m/s2
Tractor: 1.0 m/s2
Quarry dumper: 1.2 m/s2

Exposure limit values and action values
For hand-arm vibration—
(a) Standardized to an eight-hour reference period, the daily exposure limit value is 5m/s2,
(b) The action value for daily exposure, based on an eight-hour reference period, is 2.5 m/s2.
For whole-body vibration—
(a) 1.15 m/s2 shall be the daily exposure limit value based on an eight-hour reference period,
(b) The daily exposure action value, based on an eight-hour reference period, will be 0.5 m/s2.
Assessment of Exposure to Vibration
Hand Arm vibration (HAV)-
(a) The assessment of exposure to hand-arm vibration is based on the calculation of the daily exposure value normalised to an eight-hour reference period A(8), expressed as the square root of the sum of the squares (rms) (total value) of the frequency-weighted acceleration values determined on orthogonal axes ahwx, ahwy, and ahwz, as defined in Chapters 4 and 5 and Annex A of ISO (International Organization for Standardization) Standard 53 (2001).
(b) The assessment of the degree of exposure may be based on an estimate derived from manufacturer-supplied information regarding the level of emission from the utilised work equipment, the observation of specific work practises, or measurement.
Whole Body Vibration (WBV)-
(a) The assessment of exposure to mechanical vibration is based on the calculation of the daily exposure A(8) expressed as equivalent continuous acceleration over an eight-hour period, calculated as the highest (rms) value, determined on three orthogonal axes (1,4awx,1,4awy, awz for a seated or standing worker), in accordance with Chapters 5, 6 and 7, Annex A and Annex B of ISO Standard 2631-1. (1997).
(b) The assessment of the degree of exposure may be based on an estimate derived from manufacturer-supplied information regarding the level of emission from the utilized work equipment and from observation of specific work practices or on measurement..
Vibration Control Measures
Actions for controlling HAV risks could include:
(a) Substitution:
(b) Equipment selection:
(c) Maintenance:
Establish suitable maintenance routines for your equipment to prevent unwanted increases in vibration regularly sharpen and replace items such as chisels and abrasive discs so that equipment is effective and employees’ exposure time is kept to a minimum.
(d) Work schedules:
Minimize the duration of vibration exposure for your staff. Arrange work so that employees are not exposed to vibration for extended, continuous periods — a series of shorter exposures is ideal. If possible, offer Work Rotation.
(e) Clothing:
When necessary, provide your personnel with protective clothing to keep them warm and dry. This will promote healthy blood flow, which should prevent the development of vibration-related disorders.
Commercially available “anti-vibration” gloves are designed to separate the wearer’s hands from the effects of vibration. There are a variety of varieties, but none of them are particularly good at reducing the frequency-weighted vibration associated with the risk of HAVS, and some of them can actually increase the vibration at certain frequencies. It is not possible to evaluate the vibration reduction provided by “anti-vibration” gloves, hence they should not be depended upon to provide protection against vibration. Nonetheless, gloves and other warm clothes can be effective for protecting vibration-exposed personnel from the cold and preserving blood circulation.
Actions for controlling WBV risks could include:
(a) Training and instructing operators and drivers to:
(b) Selecting appropriate equipment for the job
(c) Keeping machinery and roads in satisfactory condition by:
Role of Health Surveillance
The goal of health surveillance is to prevent or swiftly diagnose any disorder associated with exposure to mechanical vibration, and it shall be deemed suitable when: —
(a) An employee’s exposure to mechanical vibration is sufficient for a measurable disease or poor health effect to be associated with the exposure,
(b) There is a realistic possibility that the sickness or harm may occur under his or her specific working settings, and
(c) The employee has access to valid, low-risk, tested approaches for detecting symptoms or effects of the condition.
References
5.3 Radiation
What is radiation?
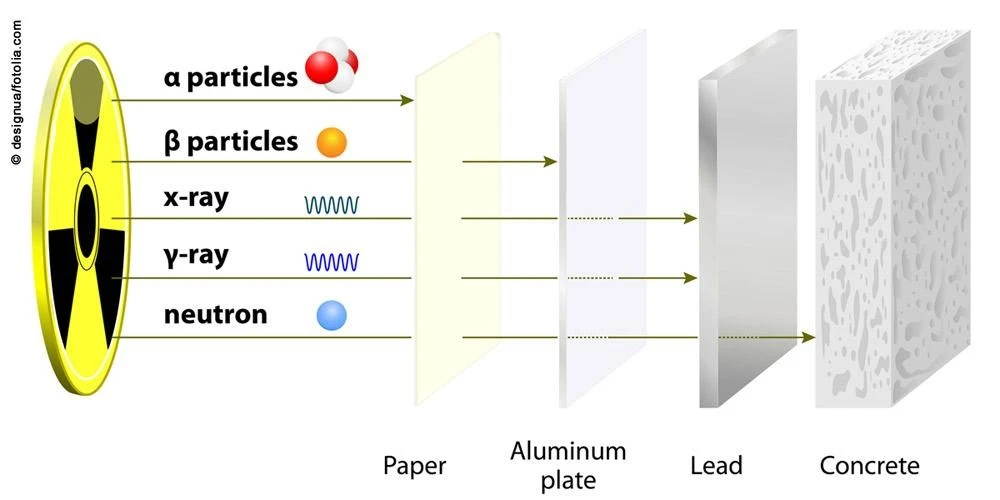
Radiation is the transmission, emission, or absorption of energy in the form of particles or waves.
Radiation exposure can be a serious occupational hazard for a range of workers. Variable effects of radiation on biological tissue.
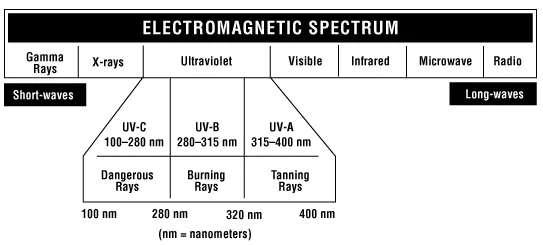
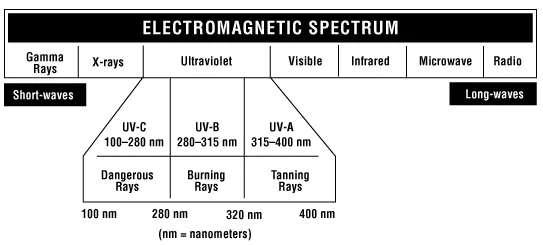
What is the difference between ionising and non-ionising radiation?
Non-ionizing radiation is distinguished from ionising radiation. Non-ionizing radiation has a longer wavelength and lower frequency, resulting in less energy. Although ionising radiation has a short wavelength and high frequency and a high energy level.
Ionising radiation: Ionizing radiation has enough energy to make ions in the molecules of matter. If that thing is a human, it can cause a lot of damage, including damage to the DNA and the breaking down of proteins. This doesn’t mean that non-ionizing radiation can’t hurt people, but it usually only causes thermal damage, like burns.
Non-ionising radiation: Many kinds of radiation, like heat, visible light, microwaves, and radio waves, don’t have enough energy to remove electrons from atoms. These kinds of radiation are called “non-ionizing radiation” because they don’t do that. In the case of heat, most of the energy is sent at infra-red wavelengths when an object is at room temperature. Ultraviolet light and lasers may still hurt your health if you are exposed to them.
Types of Non-Ionizing Radiation and Their Health Effects
This list is in order of lowest to highest frequency
Radiofrequency and Microwave Frequency Exposures
Occupational Exposures Equipment for radar and communication, industrial and commercial ovens.
Other Exposures
Cell Phones
Clinical Effects
There is a lot of disagreement about possible cancer risks, especially when it comes to cell phone use. We know that radio and microwave frequency sources can cause burns, and this is what is most likely to happen in a clinical setting.
LASER (Light Amplification by Stimulated Emission of Radiation)
Laser effects on the eye
The eye of an unprotected person is very sensitive to laser radiation, and direct or reflected beams can cause permanent damage.
Due to the way tissue works, the wavelength of the laser beam that hits the eye determines what part of the eye is hurt. Most eye damage happens to the retina, cornea, and lens.
Laser effects on the skin
The most common type of damage to the skin caused by a laser is a burn. Thermal damage is usually caused by lasers that have exposure times longer than 10 microseconds and work in the near-ultraviolet to far-infrared wavelength range.
Infrared
Common Sources
Sunlight and fire are two common natural sources. Heaters and infrared lamps, which are used in homes and infrared saunas for health reasons, are two common artificial sources. In the infrared range are also heat sources like making steel or iron and working in a foundry.
Health Effects of Infrared Radiation
IR can pass through human skin and the eye at a variety of depths, from a few millimetres for IR-A to only a few microns for IR-C. Humans have innate defensive aversion reactions to high heat pain and the intense light that is frequently present in order to prevent possibly dangerous exposure. The damaging effects of IR on human health are caused by thermal damage to tissues, which is mostly mediated by water molecules but also by modifications to protein structure. The cornea, iris, lens, and retina are all extremely vulnerable to different types of heat injury.
After repeated exposure to severe heat, lens proteins can aggregate, causing lens opacities or cataracts, as is commonly observed in glass workers and iron and steel workers.
IR intensity and duration can cause hyperthermia-related skin damage. Skin injury takes several hours at 44°C. At 70°C, this takes less than a second. After years of skin exposure to open fires, long-term IR radiation without burning can induce red-brown mottling.
Ultraviolet Radiation (UV Radiation)
In all physical respects, ultraviolet (UV) radiation is equivalent to visible light, with the exception that it does not allow us to perceive objects. Visible light, which is made up of the colours we see in a rainbow, is the kind of light that allows us to see things. After the violet end of the rainbow, the ultraviolet region begins.
Sources of UV Radiation
The main source of UV radiation is sunlight. A few different types of UV lamps, arc welding, and mercury vapour lamps are examples of artificial ultraviolet sources.
Many applications of UV radiation are found in industrial operations as well as in the fields of medicine and dentistry, including phototherapy, sun tanning, the production of fluorescent effects, the curing of inks and resins, and the death of microorganisms. For various applications, different UV wavelengths and intensities are used.
Health effects of UV Radiation
Some exposure to UV light is important for good health. It gets the body to make more vitamin D. UV lamps are one example of a medical tool that can be used to treat psoriasis (a condition causing itchy, scaly red patches on the skin).
UV radiation can cause different kinds of skin cancer, sunburn, and ageing of the skin faster. It can also cause cataracts and other eye diseases. How bad the effect is depends on the wavelength, the strength, and the length of exposure.
UV light is especially dangerous to the eyes. Even a few seconds of exposure can cause photokeratitis and conjunctivitis, which are painful but only last for a short time. Photokeratitis is a painful condition that happens when the cornea of the eye gets inflamed. The eye is watering and it’s hard to see.
UV exposure can cause eye problems like “flash burn,” “ground-glass eyeball,” “welder’s flash,” and “snow blindness,” depending on where the UV light came from that caused the injury. Pain, a feeling like there is sand in the eye, and a dislike of bright light are all signs.
Precautions
UV radiation can’t be seen, so it doesn’t make the eyes’ natural defenses work harder. When working with UV radiation sources that could cause damage to the eyes, workers must protect their eyes and skin. The type and strength of the UV source will determine what kind of eye protection you need.
UV light is easily absorbed by many different kinds of materials. Most shields are easy to design. Mercury lamps and metal halide lamps have a glass cover on the outside to stop UV radiation from getting in. If the glass cover breaks, the lamp stops working.
Types of Ionising Radiation
Sources of Ionising Radiation
Health Effects of Ionizing Radiation
When ionising radiation comes into contact with cells, it can harm the cells and their DNA (i.e., deoxyribonucleic acid, or DNA). If this damage isn’t fixed right away, it can kill the cell or cause harmful changes in the DNA (called “mutations”).
There are two kinds of health effects from radiation doses: those that can be predicted and those that can’t. Effects are definite once a certain dose is reached, which means that doses below the threshold are not likely to cause the effect. The effect gets stronger as the dose goes up. Reddening of the skin, or erythema, is one example. Even though this may not be a good way to describe all deterministic health effects, it is sometimes used to describe them.
Chance is what causes stochastic effects. The effect is more likely to happen in a population if more people get the dose, but the dose doesn’t affect how bad the effect is. Cancer is the main random effect that can come from a high dose of radiation, and it can happen many years after the exposure. It is thought that random health effects don’t have a minimum dose below which they don’t happen.
Control Measures
The role of Health Surveillance
Medical health surveillance is meant to protect workers and people who want to work for them from health risks;
(a) By making sure that people who work with radiation are fit to do their jobs as classified workers.
(b) By looking for conditions that might have the same effects as radiation.
(c) By finding conditions that might have been caused by radiation or made worse by it.
References
https://www.aocopm.org/assets/documents/10-31-11_Basic_Course_III_Orlando/ionizing%20an%20non.pdf
https://www.ccohs.ca/oshanswers/phys_agents/ultravioletradiation.html
https://www.osha.gov/ionizing-radiation
https://www.nuklearesicherheit.de/en/science/physics/ionising-radiation/types-of-ionising-radiation/
https://www.osha.gov/ionizing-radiation/control-prevention
https://www.osha.gov/ionizing-radiation/health-effects
https://inis.iaea.org/collection/NCLCollectionStore/_Public/20/052/20052336.pdf
5.4 MENTAL ILL-HEALTH
Mental Ill-Health
People with mental health problems can get better and feel more confident and socially functional if they have good jobs.
Safe and healthy workplaces are not only a basic right, but they are also more likely to reduce tension and conflicts at work and improve staff retention, work performance, and productivity. On the other hand, a lack of effective structures and support at work, especially for people with mental health problems, can make it hard for people to enjoy their jobs and do them well. It can also make people less likely to go to work or even stop them from getting a job.
Risks to mental health at work
Risks to mental health at work, also called “psychosocial risks,” can be caused by, among other things, the nature of the job or the work schedule, the way the workplace is set up, or the opportunities for career growth.
Risks to mental health at work can include:
Even though there are psychosocial risks in every industry, some workers are more likely to face them because of what they do or where and how they work. Health, humanitarian, and emergency workers are often more likely to be exposed to bad things at work, which can be bad for their mental health.
Economic downturns or public health and humanitarian crises can cause risks like job loss, financial instability, fewer job opportunities, or more unemployment.
Work can make bigger problems that hurt mental health worse, such as discrimination and inequality based on race, sex, gender identity, sexual orientation, disability, social origin, migrant status, religion, or age.
People with serious mental health problems are more likely to be turned down for jobs and more likely to face discrimination at work if they do get a job. Not having a job can also be bad for your mental health. Suicide attempts are more likely if someone is unemployed, worried about their job or finances, or just lost their job.
Element 5: Physical and psychological health
5.1 NOISE Page No. 4-13
5.2 VIBRATION Page No. 13-17
5.3 RADIATION Page No. 18-23
5.4 MENTAL ILL-HEALTH Page No. 24-31
5.5 VIOLENCE AT WORK Page No. 31-34
5.6 SUBSTANCE ABUSE AT WORK Page No. 35-37
NOISE
Scope of Learning
The physical and psychological effects of exposure to noise
The most common physical effects from Noise are as follows-
Psychological effects include-

Glossary of Terms
Sound Pressure Level- The instantaneous acoustic pressure is the sound pressure level (Lp or SPL), which is measured in decibels (dB). Since the ear is more sensitive to changes in pressure than to the power or intensity of the source, measuring this parameter shows how it affects people.
Frequency- Frequency is the number of times something happens in one second. It is measured in Hertz (Hz). For sounds, this is what people call pitch.
Decibel- It is estimated that 2 x 105 Pascals (Pa) to 200Pa is the audible sound pressure range. The range is simplified to zero decibels (dB) to one hundred forty decibels (dB) when expressed in dB notation.
A-Weighting– The human ear doesn’t react the same way to all frequencies. Most of the time, A-weighting is used to imitate how the ear responds to different frequencies. It is used to figure out how likely it is that noise will damage your hearing. It is usually written with a capital A in the unit abbreviation (e.g., LAmax, LAeq, etc.) or in brackets after a dB level (e.g., 3dB(A)).
C-Weighting– A common filter that changes the levels of a frequency spectrum in the same way that the human ear does when it hears loud or sudden noises. Most of the time, this weighting is used to judge how something sounds.
Noise Dose– A worker’s total average time-weighted exposure to noise over an 8-hour work day. This is shown as a percentage of the total amount of noise that can be heard. A noise dosimeter can be used to measure noise dose if the worker is exposed to different noise levels at different times of the day. Without a dosimeter, it can be hard to figure out the overall noise dose for different noise levels because you can’t just average the decibel levels. (A logarithmic scale is used to measure noise levels.) Not everyone agrees on the amount of noise that is safe.
Noise Exposure Levels
Why measure Noise at the Workplace?
The most important part of a program to protect workers’ hearing and reduce noise at work is measuring noise levels and workers’ exposure to noise. It helps find places of work with noise problems, employees who may be exposed to noise levels that can cause hearing loss, and places where more noise measurements need to be done. This information also helps figure out what kind of noise-control measures need to be taken.
How is workplace Noise measured?
The sound pressure level is measured to figure out noise exposures for the sake of occupational hygiene. There are many tools and methods that can be used. Which one you choose depends on how loud your workplace is and what information you need. But the first thing to do is figure out if there is a noise problem at work.
How do you identify noise problems in the workplace?
The first step is to figure out if noise could be a problem at your workplace or not. It’s best to do a walk-through survey. Some signs of a potentially dangerous noise level are:
Noise measurement results from research conducted in comparable circumstances are quite useful for identifying the potential noise problem.
What things do you consider when planning noise measurement?
When taking measurements in the field, it is essential to define the type of information needed. The individual making the measurement must comprehend:
The initial measurements are noise surveys to determine if:
The second step is to figure out each employee’s personal noise exposure level, or how much noise they are exposed to. If the noise level at work stays the same throughout the shift and the measurements are representative of a typical day, the data from the noise survey can be used to figure out if there is a risk of exposure to harmful noise levels and if more measurements are needed. But noise dosimetry, like personal noise exposure measurements, is needed if the noise level in the workplace changes during the day or if the workers move around a lot.
What types of instruments are used for measuring noise?
Most of the time, a sound level metre (SLM), an integrating sound level metre (ISLM), or a noise dosimeter is used to measure noise. It’s important to know how to calibrate, use, and read the instrument you are using. Most of this information is in the user’s manual that comes with the instrument.
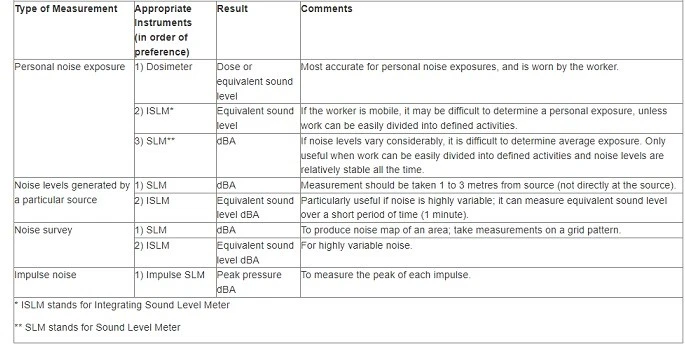
What is a noise dosimeter?
A noise dosimeter is a small, light device that the worker wears with the microphone close to their ear, just above the edge of their shoulder. The noise level information is stored in the dosimeter, which also does an averaging process. It is useful in industries where noise changes in length and volume and where people move around a lot.
A noise dosimeter requires the following settings:
(a) Level of Criteria: 8 hours a day, five days a week is the most time you can be exposed to it. In many places, the criterion level is 85 dBA, but it is 90 dBA in Quebec and 87 dBA in federal Canadian places. The OSH Answers document has more information about the levels of exposure. Limits for noise exposure at work in Canada.
(b) The noise regulation says that the exchange rate is 3 dB or 5 dB..
(c) Threshold: The lowest level of noise at which the dosimeter stops collecting noise dose data.
When a person wears the dosimeter for a full work shift, the average amount of noise exposure, or noise dose, for that person is calculated. Most of the time, this is shown as a noise exposure level, Lex,T. This is a logarithm that takes into account both how much time was actually worked and how much time was exposed. In the past, it was usually given as a percentage of the most it could be exposed to. If a person gets a noise dose of 100% over the course of a work shift, this means that the average amount of noise exposure is the most that can be allowed. For example, if the criterion level is 90 dBA and the exchange rate is 3 dBA, then being exposed to 90 dBA for eight hours gives a 100% dose. A noise dose of 100% is also 93 dBA for four hours. However, 93 dBA for eight hours is a noise dose of 200%.
Noise Action Levels
The Control of Noise at Work Regulations 2005 (Noise Regulations 2005) say that employers must prevent or reduce health and safety risks caused by noise at work. The Regulations also say that employees have to do things.
Under the Noise Regulations, you have to do certain things at certain action levels. These are about:
How much noise your employees are exposed to on average during a work day or week, and how much noise they are exposed to at their loudest (peak sound pressure) during a work day.
The values are:
Lower exposure action values:
Upper exposure action values:
The rest of the employers’ websites will tell you what you need to do. Figure 1’s flow chart will also help you figure out what you need to do.
There are also limits to how much noise someone can be around. These are called exposure limit values:
140 dB peak sound pressure (C)
Noise Control Measures
Once the risk of noise has been assessed, the next step is to control the risks.
Based on the noise levels found in the noise survey, the hierarchy of control is used to find practical and effective ways to control risks at work. Elimination or replacement of noise sources, group noise control through engineering and work organisation, and personal protective equipment make up the hierarchy of noise control (PPE).
There are many ways to keep noise down, and these will vary from workplace to workplace. There is no one method or solution that works in every circumstance. To figure out the best way to get rid of, reduce, or control the noise, you need to know a lot about what it is, where it comes from, how the plant works, what the workers do, and when they do it.
Factors the organization should consider include:
An important result of a noise risk assessment is finding ways to control the risks and putting them in order of importance. Managers should use the results of the risk assessment to make a formal plan for getting rid of noise. Among the most important steps:
Elimination
Elimination is the best way to keep workers from getting hurt because it gets rid of the noise where it comes from. This isn’t always possible, but some ways to do it would be to stop hard objects or surfaces from hitting each other or to move noisy work away from other tasks.
To cut down on nose at work, it’s important to plan and implement a good buying or renting policy. The most cost-effective and long-term way for a business to lower noise levels is to think early on about how a new work process or piece of equipment would work without making the workers too loud. Before buying new machinery, you should think about how loud it is. You can do this by talking to the manufacturer or supplier of the plant or machinery and getting information from them. This could include how to set up the machine, how to take care of it, and how loud it is likely to be in the conditions where it will be used. Note: Noise levels should always be taken into account when introducing a new work process, choosing new work equipment, or arranging the workstations.
Substitution
Substitution is the process of replacing loud machines or tools with ones that aren’t as loud. When it’s not possible to get rid of the noise-making machinery or equipment, replacing it with quieter ones may be the next best thing to do.
Organizations should always think of different tools and ways of doing work that would make the job less noisy.
Changing the way a job is done can protect the workers by making less noise. For example, using hydraulics to bend materials makes less noise than hammering.
When welding is used instead of riveting, for example, a risk assessment must be done to make sure that it doesn’t introduce a new type of risk.
Engineering controls
Engineering controls are all about making changes to processes, machines, or equipment so that workers are exposed to less noise. For example, workers can be less exposed to noise by using screens, barriers, enclosures, and materials that absorb sound.
Some engineering measures that may be considered are:
Putting more space between the noise source and the factory floor can help.
Administrative controls
Organizing tasks in such a way that fewer workers are exposed to noise for longer periods of time is an example of an administrative control. When eliminating, relocating, or retrofitting sources of noise is not an option, administrative controls should be implemented to decrease exposure levels.
Some administration controls include:
Personal protective equipment
The European Union (EU) uses a single number rating (SNR) for hearing protection, while the United States uses a noise reduction rating (NNR). As a measure of the noise reduction experienced by the wearer, this value in decibels is provided. The average person using an earmuff will experience a reduction in sound pressure of 22–33 dB, while the average person using foam earplugs will experience a reduction of 20–30 dB.
In some situations, the SNR levels won’t be high enough to keep the noise down to a manageable level. As such, new forms of management should be looked upon to reduce workers’ exposure. Workers who are always on the go, like maintenance staff, may find this challenging. Contact industry-specific specialised consultants or organisations for more help on protecting these people, since they will have a wealth of knowledge on how to regulate and manage exposure in the relevant settings.
Correct use of hearing protection is essential for its effectiveness. To ensure the success of HPE training, it is important to test employees’ comprehension of the material thereafter.
Health surveillance
What is health surveillance?
Health surveillance for hearing damage usually means:
Providing health surveillance
You must do health checks (hearing tests) on all of your employees who are likely to be exposed above the upper exposure action values on a regular basis or who are at risk for any reason, like if they already have hearing loss or are more likely to get hurt.
The purpose of health surveillance is to:
References
https://www.hear-it.org/temporary-threshold-shift
https://en.wikipedia.org/wiki/Health_effects_from_noise
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1637786/pdf/envhper00310-0128.pdf https://www.transport.gov.scot/media/6954/app-a8_1-noise-and-vibration-terminology.pdf
http://www.larsondavis.com/learn/sound-vibe-basics/sound-measurement-terminology
https://kb.q-windows.com/benefit/soundproof-aluminum-windows-doors
https://www.ccohs.ca/oshanswers/phys_agents/noise_measurement.html
https://www.hse.gov.uk/noise/employers.htm
https://www.hse.gov.uk/noise/healthsurveillance.htm#what
5.2 VIBRATION
The effects on the body of exposure to hand–arm vibration and whole-body vibration
Mechanical vibrations at work can expose workers to hand-arm vibration (HAV) and/or whole-body vibration (WBV).
Hand Arm Vibration (HAV)- HAV is caused by using tools and doing tasks at work that send vibrations into the hands and arms of workers. It can be caused by hand-held power tools like hammer drills, sanders, grinders, and concrete breakers; hand-guided equipment like powered lawnmowers, chainsaws, and hedge trimmers; or by holding materials being worked on by machines like bench-mounted grinders, pedestal grinders, etc.
Hand-arm vibration syndrome (HAVS) is a group of health problems that can be caused by long-term, regular exposure to HAV. Some of these problems, like vibration white finger and carpal tunnel syndrome, can be permanent and painful..
HAVS affects the hand, wrist, and arm’s nerves, blood vessels, muscles, and joints. If you don’t take care of it, it can make you very sick. Carpal tunnel syndrome is a disorder of the nerves in the wrist that can cause pain, tingling, numbness, and weakness in the hand and wrist. It can happen on its own, but vibration is one of the things that can cause it. Early signs of a problem include tingling and numbness, not being able to feel things with your fingers, losing strength in your hands, and having white fingers that turn red and hurt when they get cold and wet.
Vibration white finger is very painful and can make it hard to move. If vibration continues, it can spread and affect more fingers. Workers who are pregnant, have diseases of the hands, arms, wrists, or shoulders, or have diseases that affect blood flow, like diabetes, are more likely to be affected by HAV. The general and heavy engineering, construction and civil engineering, forestry, and horticulture industries are all connected to HAV.
Whole Body Vibration (WBV)- WBV is caused by machines and vehicles at work that send vibrations up through the seat or down through the feet. It can be caused by driving off-road vehicles, like tractors, over rough surfaces. It can also be caused by excavators digging into hard ground, or by standing close to powerful machines that aren’t moving.
Low back pain has been linked to long-term exposure to high levels of WBV. People who are more likely to be sensitive to WBV include workers who are pregnant, people with neck or back problems, young people whose bones and muscles are not fully developed, and people who have just had surgery. Mining, building, and farming are all industries that work with WBV.
The amount of vibration a person is exposed to is measured by how fast the surface they are in contact with is moving. Most of the time, the speed of the surface is measured in metres per second squared (m/s2).
An accelerometer is a device that is attached to the surface that is moving and gives an output that is proportional to the acceleration. After the frequency weighting has been used, the average size of the vibration is shown.
Typical vibration magnitudes for equipment used at work are as follows.
For HAV:
Chainsaw: 6 m/s2
Sander: 8 m/s2
Hammer drill: 9 m/s2
Road breaker: 12 m/s2
For WBV:
Car: 0.4 m/s2
Lorry: 0.7 m/s2
Tractor: 1.0 m/s2
Quarry dumper: 1.2 m/s2

Exposure limit values and action values
For hand-arm vibration—
(a) Standardized to an eight-hour reference period, the daily exposure limit value is 5m/s2,
(b) The action value for daily exposure, based on an eight-hour reference period, is 2.5 m/s2.
For whole-body vibration—
(a) 1.15 m/s2 shall be the daily exposure limit value based on an eight-hour reference period,
(b) The daily exposure action value, based on an eight-hour reference period, will be 0.5 m/s2.
Assessment of Exposure to Vibration
Hand Arm vibration (HAV)-
(a) The assessment of exposure to hand-arm vibration is based on the calculation of the daily exposure value normalised to an eight-hour reference period A(8), expressed as the square root of the sum of the squares (rms) (total value) of the frequency-weighted acceleration values determined on orthogonal axes ahwx, ahwy, and ahwz, as defined in Chapters 4 and 5 and Annex A of ISO (International Organization for Standardization) Standard 53 (2001).
(b) The assessment of the degree of exposure may be based on an estimate derived from manufacturer-supplied information regarding the level of emission from the utilised work equipment, the observation of specific work practises, or measurement.
Whole Body Vibration (WBV)-
(a) The assessment of exposure to mechanical vibration is based on the calculation of the daily exposure A(8) expressed as equivalent continuous acceleration over an eight-hour period, calculated as the highest (rms) value, determined on three orthogonal axes (1,4awx,1,4awy, awz for a seated or standing worker), in accordance with Chapters 5, 6 and 7, Annex A and Annex B of ISO Standard 2631-1. (1997).
(b) The assessment of the degree of exposure may be based on an estimate derived from manufacturer-supplied information regarding the level of emission from the utilized work equipment and from observation of specific work practices or on measurement..
Vibration Control Measures
Actions for controlling HAV risks could include:
(a) Substitution:
(b) Equipment selection:
(c) Maintenance:
Establish suitable maintenance routines for your equipment to prevent unwanted increases in vibration regularly sharpen and replace items such as chisels and abrasive discs so that equipment is effective and employees’ exposure time is kept to a minimum.
(d) Work schedules:
Minimize the duration of vibration exposure for your staff. Arrange work so that employees are not exposed to vibration for extended, continuous periods — a series of shorter exposures is ideal. If possible, offer Work Rotation.
(e) Clothing:
When necessary, provide your personnel with protective clothing to keep them warm and dry. This will promote healthy blood flow, which should prevent the development of vibration-related disorders.
Commercially available “anti-vibration” gloves are designed to separate the wearer’s hands from the effects of vibration. There are a variety of varieties, but none of them are particularly good at reducing the frequency-weighted vibration associated with the risk of HAVS, and some of them can actually increase the vibration at certain frequencies. It is not possible to evaluate the vibration reduction provided by “anti-vibration” gloves, hence they should not be depended upon to provide protection against vibration. Nonetheless, gloves and other warm clothes can be effective for protecting vibration-exposed personnel from the cold and preserving blood circulation.
Actions for controlling WBV risks could include:
(a) Training and instructing operators and drivers to:
(b) Selecting appropriate equipment for the job
(c) Keeping machinery and roads in satisfactory condition by:
Role of Health Surveillance
The goal of health surveillance is to prevent or swiftly diagnose any disorder associated with exposure to mechanical vibration, and it shall be deemed suitable when: —
(a) An employee’s exposure to mechanical vibration is sufficient for a measurable disease or poor health effect to be associated with the exposure,
(b) There is a realistic possibility that the sickness or harm may occur under his or her specific working settings, and
(c) The employee has access to valid, low-risk, tested approaches for detecting symptoms or effects of the condition.
References
5.3 Radiation
What is radiation?
Radiation is the transmission, emission, or absorption of energy in the form of particles or waves.
Radiation exposure can be a serious occupational hazard for a range of workers. Variable effects of radiation on biological tissue.
What is the difference between ionising and non-ionising radiation?
Non-ionizing radiation is distinguished from ionising radiation. Non-ionizing radiation has a longer wavelength and lower frequency, resulting in less energy. Although ionising radiation has a short wavelength and high frequency and a high energy level.
Ionising radiation: Ionizing radiation has enough energy to make ions in the molecules of matter. If that thing is a human, it can cause a lot of damage, including damage to the DNA and the breaking down of proteins. This doesn’t mean that non-ionizing radiation can’t hurt people, but it usually only causes thermal damage, like burns.
Non-ionising radiation: Many kinds of radiation, like heat, visible light, microwaves, and radio waves, don’t have enough energy to remove electrons from atoms. These kinds of radiation are called “non-ionizing radiation” because they don’t do that. In the case of heat, most of the energy is sent at infra-red wavelengths when an object is at room temperature. Ultraviolet light and lasers may still hurt your health if you are exposed to them.
Types of Non-Ionizing Radiation and Their Health Effects
This list is in order of lowest to highest frequency
Radiofrequency and Microwave Frequency Exposures
Occupational Exposures Equipment for radar and communication, industrial and commercial ovens.
Other Exposures
Cell Phones
Clinical Effects
There is a lot of disagreement about possible cancer risks, especially when it comes to cell phone use. We know that radio and microwave frequency sources can cause burns, and this is what is most likely to happen in a clinical setting.
LASER (Light Amplification by Stimulated Emission of Radiation)
Laser effects on the eye
The eye of an unprotected person is very sensitive to laser radiation, and direct or reflected beams can cause permanent damage.
Due to the way tissue works, the wavelength of the laser beam that hits the eye determines what part of the eye is hurt. Most eye damage happens to the retina, cornea, and lens.
Laser effects on the skin
The most common type of damage to the skin caused by a laser is a burn. Thermal damage is usually caused by lasers that have exposure times longer than 10 microseconds and work in the near-ultraviolet to far-infrared wavelength range.
Infrared
Common Sources
Sunlight and fire are two common natural sources. Heaters and infrared lamps, which are used in homes and infrared saunas for health reasons, are two common artificial sources. In the infrared range are also heat sources like making steel or iron and working in a foundry.
Health Effects of Infrared Radiation
IR can pass through human skin and the eye at a variety of depths, from a few millimetres for IR-A to only a few microns for IR-C. Humans have innate defensive aversion reactions to high heat pain and the intense light that is frequently present in order to prevent possibly dangerous exposure. The damaging effects of IR on human health are caused by thermal damage to tissues, which is mostly mediated by water molecules but also by modifications to protein structure. The cornea, iris, lens, and retina are all extremely vulnerable to different types of heat injury.
After repeated exposure to severe heat, lens proteins can aggregate, causing lens opacities or cataracts, as is commonly observed in glass workers and iron and steel workers.
IR intensity and duration can cause hyperthermia-related skin damage. Skin injury takes several hours at 44°C. At 70°C, this takes less than a second. After years of skin exposure to open fires, long-term IR radiation without burning can induce red-brown mottling.
Ultraviolet Radiation (UV Radiation)
In all physical respects, ultraviolet (UV) radiation is equivalent to visible light, with the exception that it does not allow us to perceive objects. Visible light, which is made up of the colours we see in a rainbow, is the kind of light that allows us to see things. After the violet end of the rainbow, the ultraviolet region begins.
Sources of UV Radiation
The main source of UV radiation is sunlight. A few different types of UV lamps, arc welding, and mercury vapour lamps are examples of artificial ultraviolet sources.
Many applications of UV radiation are found in industrial operations as well as in the fields of medicine and dentistry, including phototherapy, sun tanning, the production of fluorescent effects, the curing of inks and resins, and the death of microorganisms. For various applications, different UV wavelengths and intensities are used.
Health effects of UV Radiation
Some exposure to UV light is important for good health. It gets the body to make more vitamin D. UV lamps are one example of a medical tool that can be used to treat psoriasis (a condition causing itchy, scaly red patches on the skin).
UV radiation can cause different kinds of skin cancer, sunburn, and ageing of the skin faster. It can also cause cataracts and other eye diseases. How bad the effect is depends on the wavelength, the strength, and the length of exposure.
UV light is especially dangerous to the eyes. Even a few seconds of exposure can cause photokeratitis and conjunctivitis, which are painful but only last for a short time. Photokeratitis is a painful condition that happens when the cornea of the eye gets inflamed. The eye is watering and it’s hard to see.
UV exposure can cause eye problems like “flash burn,” “ground-glass eyeball,” “welder’s flash,” and “snow blindness,” depending on where the UV light came from that caused the injury. Pain, a feeling like there is sand in the eye, and a dislike of bright light are all signs.
Precautions
UV radiation can’t be seen, so it doesn’t make the eyes’ natural defenses work harder. When working with UV radiation sources that could cause damage to the eyes, workers must protect their eyes and skin. The type and strength of the UV source will determine what kind of eye protection you need.
UV light is easily absorbed by many different kinds of materials. Most shields are easy to design. Mercury lamps and metal halide lamps have a glass cover on the outside to stop UV radiation from getting in. If the glass cover breaks, the lamp stops working.
Types of Ionising Radiation
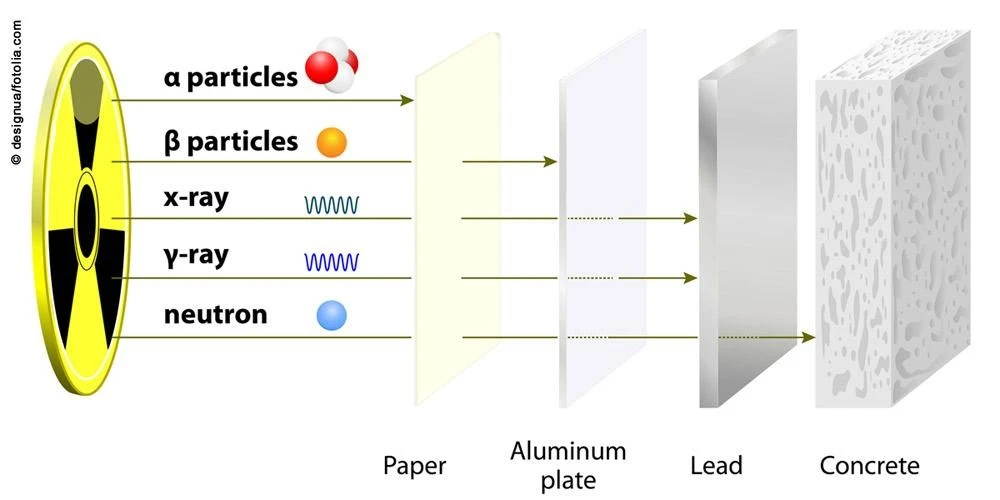
Sources of Ionising Radiation
Health Effects of Ionizing Radiation
When ionising radiation comes into contact with cells, it can harm the cells and their DNA (i.e., deoxyribonucleic acid, or DNA). If this damage isn’t fixed right away, it can kill the cell or cause harmful changes in the DNA (called “mutations”).
There are two kinds of health effects from radiation doses: those that can be predicted and those that can’t. Effects are definite once a certain dose is reached, which means that doses below the threshold are not likely to cause the effect. The effect gets stronger as the dose goes up. Reddening of the skin, or erythema, is one example. Even though this may not be a good way to describe all deterministic health effects, it is sometimes used to describe them.
Chance is what causes stochastic effects. The effect is more likely to happen in a population if more people get the dose, but the dose doesn’t affect how bad the effect is. Cancer is the main random effect that can come from a high dose of radiation, and it can happen many years after the exposure. It is thought that random health effects don’t have a minimum dose below which they don’t happen.
Control Measures
The role of Health Surveillance
Medical health surveillance is meant to protect workers and people who want to work for them from health risks;
(a) By making sure that people who work with radiation are fit to do their jobs as classified workers.
(b) By looking for conditions that might have the same effects as radiation.
(c) By finding conditions that might have been caused by radiation or made worse by it.
References
https://www.aocopm.org/assets/documents/10-31-11_Basic_Course_III_Orlando/ionizing%20an%20non.pdf
https://www.ccohs.ca/oshanswers/phys_agents/ultravioletradiation.html
https://www.osha.gov/ionizing-radiation
https://www.nuklearesicherheit.de/en/science/physics/ionising-radiation/types-of-ionising-radiation/
https://www.osha.gov/ionizing-radiation/control-prevention
https://www.osha.gov/ionizing-radiation/health-effects
https://inis.iaea.org/collection/NCLCollectionStore/_Public/20/052/20052336.pdf
5.4 MENTAL ILL-HEALTH
Mental Ill-Health
People with mental health problems can get better and feel more confident and socially functional if they have good jobs.
Safe and healthy workplaces are not only a basic right, but they are also more likely to reduce tension and conflicts at work and improve staff retention, work performance, and productivity. On the other hand, a lack of effective structures and support at work, especially for people with mental health problems, can make it hard for people to enjoy their jobs and do them well. It can also make people less likely to go to work or even stop them from getting a job.
Risks to mental health at work
Risks to mental health at work, also called “psychosocial risks,” can be caused by, among other things, the nature of the job or the work schedule, the way the workplace is set up, or the opportunities for career growth.
Risks to mental health at work can include:
Even though there are psychosocial risks in every industry, some workers are more likely to face them because of what they do or where and how they work. Health, humanitarian, and emergency workers are often more likely to be exposed to bad things at work, which can be bad for their mental health.
Economic downturns or public health and humanitarian crises can cause risks like job loss, financial instability, fewer job opportunities, or more unemployment.
Work can make bigger problems that hurt mental health worse, such as discrimination and inequality based on race, sex, gender identity, sexual orientation, disability, social origin, migrant status, religion, or age.
People with serious mental health problems are more likely to be turned down for jobs and more likely to face discrimination at work if they do get a job. Not having a job can also be bad for your mental health. Suicide attempts are more likely if someone is unemployed, worried about their job or finances, or just lost their job.
Serious Signs of Mental Health Issues
If you think one of your employees is having a mental health problem, you should act quickly. Early intervention is important for both the health of the worker and the health of your business. If you see any of these important signs, it may be time to step in:
What is stress?
Stress, according to the Health and Safety Executive (HSE), is “the bad reaction people have to too much pressure or other types of demand placed on them.”
When people at work can’t deal with pressures and other problems, they feel stressed. Employers should match their needs with the skills and knowledge of their workers. For example, workers can feel stressed if they don’t think they have the skills or time to meet tight deadlines. Planning, training, and help can help relieve pressure and lower stress levels.
People react differently to stress, so what stresses one person might not stress another. Whether or not a worker can deal with a situation depends on skills, experience, age, or a disability.
Six main parts of how a job is set up can affect how stressful it is. You should take care of these well. They are:
Employers should assess the risks in these areas to manage stress in the workplace.
What are the Management Standards for work-related stress?
The Management Standards describe the traits or culture of an organisation that effectively manages and controls the risks that come from work-related stress.
They cover six important parts of how work is set up that, if not managed well, can lead to bad health and well-being, lower productivity, and more sick days. In other words, the six Management Standards cover the main things at work that cause stress. These things:
■ Demands – This includes things like the amount of work, the schedule, and the environment at work.
■ Control – how much control a person has over how they do their job.
■ Support – This includes the support, encouragement, and resources given by the company, line management, and colleagues.
■ Relationships – This includes encouraging good work to avoid conflict and dealing with behaviour that isn’t acceptable.
■ Role – if people know what their role is in the organisation and if the organisation makes sure that people don’t have roles that are at odds with each other.
■ Change – how big or small organisational changes are handled and shared in the organisation.The Management Standards
In the “What should be happening/States to be achieved” section of each Standard, there is a list of good things that organisations should try to achieve.
The six Management Standards are:
Demands
Includes issues like workload, work patterns, and the work environment.
The Standard is that:
■ Employees say they can handle the requirements of their jobs; and
■ Locally, there are ways to handle any individual concerns..
What should be happening/States to be achieved?
■ the company gives workers reasonable and doable tasks to do during their agreed-upon hours of work;
■ The skills and abilities of people are matched to the needs of the job;
■ Jobs are made to fit the skills of the people who do them; and
■ The problems that employees have with their work environment are dealt with.
Control
How much say the person has in the way they do their work.
The Standard is that:
■ Employees say they have a say in how they do their jobs; and
■ Locally, there are ways to handle any individual concerns.
What should be happening/States to be achieved?
■ When it’s possible, employees are in charge of how fast they work;
■ Employees are encouraged to do their jobs using their skills and initiative;
■ When it’s possible, employees are encouraged to learn new skills that will help them take on new and hard tasks;
■ the company encourages its workers to improve their skills;
■ Employees get to decide when they can take breaks;
■ Employees are asked about their work schedules..
Support
Includes the support, sponsorship, and resources that the organisation, line management, and other colleagues gave.
The Standard is that:
■ Employees say that their coworkers and bosses provide them with enough information and help; and
■ Locally, there are ways to handle any individual concerns.
What should be happening/States to be achieved?
■ the company has policies and procedures in place to help its workers;
■ There are systems in place that make it possible for and encourage managers to help their staff;
■ There are systems in place that allow and encourage employees to help each other;
■ Employees know what kind of help is available, how to get it, and when;
■ Workers know how to get to the tools they need to do their jobs; and
■ Regular and helpful feedback is given to employees.
Relationships
Includes encouraging good work to avoid conflict and dealing with behaviour that isn’t acceptable.
The Standard is that:
■ Employees say they are not bullied or treated in any other way that is not acceptable at work; and
■ Locally, there are ways to handle any individual concerns..
What should be happening/States to be achieved?
■ the company encourages good behavior at work to avoid conflicts and make sure everyone gets treated fairly;
■ Employees talk about things that are important to their jobs;
■ the organization has policies and procedures in place to stop or fix behavior that is not acceptable;
■ There are systems in place that make it easy for and encourage managers to deal with bad behavior;
■ There are systems in place that make it easy for employees to report bad behavior and encourage them to do so.
Role
If people know what their role is in the organization and if the organization makes sure that people don’t have roles that conflict with each other.
The Standard is that:
■ Employees say they know what their role is and what their responsibilities are; and
■ Locally, there are ways to handle any individual concerns.
What should be happening/States to be achieved?
■ The company tries to make sure that the different requirements it has for its employees work together as much as possible;
■ the company gives employees information about their roles and responsibilities so they can understand them;
■ the company makes sure that the requirements it has for its employees are as clear as possible; and
■ It is possible for employees to express their concerns on any ambiguities or conflicts in their roles and duties through the use of established procedures.
Change
How organizational change (large or small) is managed and communicated in the organization.
The Standard is that:
■ Workers report that the organization frequently engages them throughout organizational transformation; and
■ Local systems are in place to address particular issues.
What should be happening/States to be achieved?
■ The organization gives employees with timely information so they may comprehend the rationale behind planned changes.
■ The company ensures proper employee consultation on changes and affords staff opportunities to influence suggestions.
■ Workers are informed of the likely consequences of any changes to their positions. Employees receive training, if necessary, to support any changes to their jobs;
■ Workers are informed of changing timelines; and
■ During transitions, employees have access to relevant support.
References
https://www.who.int/news-room/fact-sheets/detail/mental-health-at-work
5.5 VIOLENCE AT WORK
What is Violence?
The Health and Safety Executive defines workplace violence as follows: (a) “any occurrence in which a person is abused, intimidated, or assaulted in work-related circumstances.”
(b) Verbal abuse and threats are the most frequent forms of violence. Physical attacks are rather uncommon.
Who is at risk?
Those whose jobs compel them to interact with the public may be vulnerable to violence. Most vulnerable are those who engage in:
■ giving a service
■ Caring
■ Education
■ Cash transactions
■ delivery/collection
■ controlling
■ representing authority
What the law requires
There are five key health and safety laws that pertain to workplace violence.
They include:
■ The Health and Safety at Work etc. Act 1974 (HSW Act)
Employers are required by law to guarantee their employees’ health, safety, and wellbeing at work, so far as is reasonably practicable.
■ The Management of Health and Safety at Work Regulations 1999
Businesses are required to evaluate the hazards to their employees and make arrangements for their health and safety by:
– planning;
– Organization;
– Control;
– Monitoring and review.
The risks should, when applicable, include the requirement to protect employees against exposure to violence that is reasonably foreseeable.
■ The Reporting of Injuries, Diseases and Dangerous Occurrences
Regulations 1995 (RIDDOR)
Employers must notify their enforcement authority in the event of a workplace accident resulting in the death of an employee, a serious injury, or incapacity for normal work for at least three consecutive days. This includes any nonconsensual act of physical assault against an employee.
■ Safety Representatives and Safety Committees Regulations 1977 (a) and
The Health and Safety (Consultation with Employees) Regulations 1996 (b)
Companies must provide employees with timely information and consultation regarding their health and safety. Employee representatives, either nominated by recognized trade unions or elected by their co-workers (a) or elected under (b) may communicate with their employer about concerns endangering the health and safety of persons they represent.
Effective management of violence at Work
A straightforward four stage management process is set out below-
Stage 1 Finding out if you have a problem
Stage 2 deciding what action to take
Stage 3 Take action
Stage 4 Check what you have done
Stage 1 Finding out if you have a problem
The first step of risk assessment is hazard identification. You may believe that workplace violence is not a problem or that incidences are uncommon. But, your staff may have a quite different perspective.
Ask your staff – Do this informally through managers, supervisors, and safety advocates, or utilize a brief survey to see if your staff ever feel endangered. Inform them of the results of your survey to demonstrate that you identify the issue.
Keep detailed records It is advisable to document instances, such as verbal abuse and threats. You may find it beneficial to jot down the following details:
■ An account of what happened;
■ details of the victim(s), the assailant(s) and any witnesses;
■ the outcome, including working time lost to both the individual(s) affected and
to the organization as a whole;
■ the details of the location of the incident.
Classify all incidents – Use headings such as location, time, event type, potential severity, parties involved, and likely causes. It is essential that you study each event report to see whether a more severe outcome could have occurred. Here is an example of a simple classification for determining the severity of incidents:
■ fatal injury;
■ major injury;
■ injury or emotional shock requiring first aid, out-patient treatment, counselling,
absence from work (record number of days);
■ feeling of being at risk or distressed.
Try to predict what might happen – Do not limit your evaluation to occurrences that have already impacted your personnel. There may be a pattern of violence associated with particular job conditions. Trade and professional organizations and labor unions may have important information regarding this. Local, national, and technical press articles may help inform you of pertinent happenings and prospective issue areas.
Stage 2 deciding what action to take
Having discovered that violence could be a concern for your staff, you must determine the appropriate course of action. Continue the risk assessment by completing the steps below, which will assist you in determining the necessary course of action.
Decide who might be harmed, and how
Identify which employees are at risk – Those that interact with the public face-to-face are typically the most susceptible. Whenever possible, identify potentially violent individuals in advance in order to limit the dangers associated with them.
Evaluate the risk
Examine the current safety precautions; are they sufficient, or should more be done? Keep in mind that violence is typically caused by a mix of causes. Variables which you can affect include:
■ the level of training and information provided;
■ the environment;
■ the design of the job.
Consider the way these factors work together to influence the risk of violence.
Training and information
Teach your employees to recognize the early warning signs of hostility so that they can either avoid or deal with it. Ensure that they completely comprehend any security measures you’ve implemented.
Give personnel with any information they may require to identify clients with a history of violence or to predict factors that may increase the likelihood of violence.
The environment
Offer improved seating, dcor, and lighting in public waiting areas, as well as more frequent updates on delays.
Consider the following physical security measures:
■ Video cameras or alarm systems;
■ coded security locks on doors to keep the public out of staff areas;
■ wider counters and raised floors on the staff side of the counter to give staff more protection.
The design of the job
Use checks, credit cards, or tokens instead of cash to reduce the appeal of robbery.
Increase the frequency of your bank visits and vary your route to lessen the chance of robbery.
Verify the credentials of clients and the location and logistics of any off-site meetings.
Arrange for employees to be escorted by a coworker if they must meet a potential aggressor at their residence or in a remote area.
Make preparations for remote personnel to stay in touch with their home office.
Sustain staffing levels to prevent a lone worker situation from arising.
Record your findings
Document the major findings of your evaluation. The document should serve as a working document for both management and staff.
Review and revise your assessment
Periodically verify that your evaluation accurately reflects your current work environment. Be willing to add additional measures or modify existing measures when they are ineffective. This is especially crucial when a job is changed. If a violent occurrence occurs, reassess your assessment and make any necessary adjustments.
Stage 3 Take action
Your policy for addressing violence could be included in your health and safety policy statement, so that all employees are aware of it. This will aid your employees in cooperating with you, adhering to protocols, and reporting additional events.
Stage 4 Check what you have done
Regularly evaluate the effectiveness of your arrangements, consulting with employees or their representatives. Consider establishing joint management and safety committees for this purpose. Maintain records of incidents and review them frequently; they will demonstrate your progress and whether the situation is evolving. If your measures are effective, maintain them.
If violence remains a problem, consider a different approach. Return to Stages 1 and 2 and discover other preventive measures that may be effective.
References-
https://www.hse.gov.uk/pubns/indg69.pdf
5.6 SUBSTANCE ABUSE AT WORK
Businesses are required by law to protect the health, safety, and welfare of their employees. Knowing the indicators of drug and alcohol misuse (or abuse) will enable you to manage health and safety risks in the workplace, create a strategy to address drug-related issues, and provide support for your staff.
What the issues are and what to look out for
Abuse is not equivalent to dependence. The use of illegal narcotics and the abuse of alcohol, pharmaceuticals, and chemicals such as solvents constitutes drug and alcohol abuse.
Consider the following indicators of substance or alcohol abuse:
How to Manage Substance Abuse Issues?
Consult your employees
Employees or their representatives must be consulted on health and safety problems. Consultation entails not only providing information to employees but also listening to and considering their feedback.
You might ask your employees about their knowledge of the consequences of drugs and alcohol on health and safety, as well as the restrictions or guidelines governing drug and alcohol usage in your workplace.
Look at safety-critical work
Consider the nature of your profession and any safety-critical aspects where drug or alcohol abuse could have severe consequences.
for example:
Develop a policy
An agreed-upon policy on drug/alcohol abuse can help all organizations. You might include a policy on drugs and alcohol in your overall health and safety policy.
An effective policy should strive to aid and support an employee who discloses a drug or alcohol issue, rather than result in termination.
But it should also indicate when you will take disciplinary or other action, such as immediately reporting drug possession or distribution to the authorities.
When personnel in safety-sensitive positions seek treatment for alcohol or drug abuse, it may be necessary to temporarily transfer them to a different position.
You could incorporate screening and testing for drugs and alcohol in your policy if you elect to do so.
Screening and testing for drugs and alcohol
Some employers have incorporated testing into their drug and alcohol policies. If you choose to do the same, you should carefully consider the purpose of screening and what you will do with the information it provides.
There may be a reason for screening, especially in specific occupations (for example employees who make safety-critical decisions like drivers, pilots and some machinery operators). In these positions, the usage of drugs or alcohol could have catastrophic consequences for the individual, his or her coworkers, the general public, and the environment.
Bear in mind that:
Support employees with a drug or alcohol problem
After assessing the risk and establishing a policy for drug or alcohol misuse (or abuse) in the workplace, ensure that your employees are aware of the policy and the support you provide.
Training and awareness
Provide a description of the drug and alcohol misuse policy in the onboarding process for all new workers to enhance awareness.
You could also brief managers and supervisors so they are clear about:
Support for employees
Workers with a drug or alcohol problem may seek assistance at work if they are assured that their issues will be handled discretely and in confidence. Consider your own legal position if proof or information indicates that an employee’s drug abuse has resulted in workplace violations.
Alcohol and drug addiction are recognized medical conditions. A person who is abusing drugs or alcohol has the same rights to privacy and assistance as someone with any other medical or psychiatric issue.
Urge them to seek assistance from their primary care physician or a specialized drug or alcohol agency, and recommend them to the occupational health department of your organization (if you have one).
Consider granting someone time off to obtain expert assistance. Frequently, the cost of hiring and training a new employee exceeds the cost of time off.
Consider whether your workplace treats drug and alcohol abuse as a disciplinary matter or a health concern. An employment tribunal may determine that you have terminated someone unfairly if you fire them for drug or alcohol abuse without attempting to help them.
But, if their typical job is safety-sensitive, you may need to temporarily transfer them to a different position.
Health advice and information
Even without occupational health services, you can still support the health and welfare of your employees. You can ensure that employees have access to information on where they can go for guidance and assistance if they are concerned about drug or alcohol abuse.
The law
Under the Health and Safety at Work etc. Act, you have a general obligation to ensure the health, safety, and welfare of your employees so far as is practically practicable. Also, employees must take reasonable care of themselves and anyone whose health may be harmed by their work. There is up-to-date information on regulations pertaining to drug and alcohol abuse, such as the Misuse of Drugs Act of 1971 and the Road Traffic Act of 1988. Frank also possesses useful legal knowledge.
References
Serious Signs of Mental Health Issues
If you think one of your employees is having a mental health problem, you should act quickly. Early intervention is important for both the health of the worker and the health of your business. If you see any of these important signs, it may be time to step in:
What is stress?
Stress, according to the Health and Safety Executive (HSE), is “the bad reaction people have to too much pressure or other types of demand placed on them.”
When people at work can’t deal with pressures and other problems, they feel stressed. Employers should match their needs with the skills and knowledge of their workers. For example, workers can feel stressed if they don’t think they have the skills or time to meet tight deadlines. Planning, training, and help can help relieve pressure and lower stress levels.
People react differently to stress, so what stresses one person might not stress another. Whether or not a worker can deal with a situation depends on skills, experience, age, or a disability.
Six main parts of how a job is set up can affect how stressful it is. You should take care of these well. They are:
Employers should assess the risks in these areas to manage stress in the workplace.
What are the Management Standards for work-related stress?
The Management Standards describe the traits or culture of an organisation that effectively manages and controls the risks that come from work-related stress.
They cover six important parts of how work is set up that, if not managed well, can lead to bad health and well-being, lower productivity, and more sick days. In other words, the six Management Standards cover the main things at work that cause stress. These things:
■ Demands – This includes things like the amount of work, the schedule, and the environment at work.
■ Control – how much control a person has over how they do their job.
■ Support – This includes the support, encouragement, and resources given by the company, line management, and colleagues.
■ Relationships – This includes encouraging good work to avoid conflict and dealing with behaviour that isn’t acceptable.
■ Role – if people know what their role is in the organisation and if the organisation makes sure that people don’t have roles that are at odds with each other.
■ Change – how big or small organisational changes are handled and shared in the organisation.The Management Standards
In the “What should be happening/States to be achieved” section of each Standard, there is a list of good things that organisations should try to achieve.
The six Management Standards are:
Demands
Includes issues like workload, work patterns, and the work environment.
The Standard is that:
■ Employees say they can handle the requirements of their jobs; and
■ Locally, there are ways to handle any individual concerns..
What should be happening/States to be achieved?
■ the company gives workers reasonable and doable tasks to do during their agreed-upon hours of work;
■ The skills and abilities of people are matched to the needs of the job;
■ Jobs are made to fit the skills of the people who do them; and
■ The problems that employees have with their work environment are dealt with.
Control
How much say the person has in the way they do their work.
The Standard is that:
■ Employees say they have a say in how they do their jobs; and
■ Locally, there are ways to handle any individual concerns.
What should be happening/States to be achieved?
■ When it’s possible, employees are in charge of how fast they work;
■ Employees are encouraged to do their jobs using their skills and initiative;
■ When it’s possible, employees are encouraged to learn new skills that will help them take on new and hard tasks;
■ the company encourages its workers to improve their skills;
■ Employees get to decide when they can take breaks;
■ Employees are asked about their work schedules..
Support
Includes the support, sponsorship, and resources that the organisation, line management, and other colleagues gave.
The Standard is that:
■ Employees say that their coworkers and bosses provide them with enough information and help; and
■ Locally, there are ways to handle any individual concerns.
What should be happening/States to be achieved?
■ the company has policies and procedures in place to help its workers;
■ There are systems in place that make it possible for and encourage managers to help their staff;
■ There are systems in place that allow and encourage employees to help each other;
■ Employees know what kind of help is available, how to get it, and when;
■ Workers know how to get to the tools they need to do their jobs; and
■ Regular and helpful feedback is given to employees.
Relationships
Includes encouraging good work to avoid conflict and dealing with behaviour that isn’t acceptable.
The Standard is that:
■ Employees say they are not bullied or treated in any other way that is not acceptable at work; and
■ Locally, there are ways to handle any individual concerns..
What should be happening/States to be achieved?
■ the company encourages good behavior at work to avoid conflicts and make sure everyone gets treated fairly;
■ Employees talk about things that are important to their jobs;
■ the organization has policies and procedures in place to stop or fix behavior that is not acceptable;
■ There are systems in place that make it easy for and encourage managers to deal with bad behavior;
■ There are systems in place that make it easy for employees to report bad behavior and encourage them to do so.
Role
If people know what their role is in the organization and if the organization makes sure that people don’t have roles that conflict with each other.
The Standard is that:
■ Employees say they know what their role is and what their responsibilities are; and
■ Locally, there are ways to handle any individual concerns.
What should be happening/States to be achieved?
■ The company tries to make sure that the different requirements it has for its employees work together as much as possible;
■ the company gives employees information about their roles and responsibilities so they can understand them;
■ the company makes sure that the requirements it has for its employees are as clear as possible; and
■ It is possible for employees to express their concerns on any ambiguities or conflicts in their roles and duties through the use of established procedures.
Change
How organizational change (large or small) is managed and communicated in the organization.
The Standard is that:
■ Workers report that the organization frequently engages them throughout organizational transformation; and
■ Local systems are in place to address particular issues.
What should be happening/States to be achieved?
■ The organization gives employees with timely information so they may comprehend the rationale behind planned changes.
■ The company ensures proper employee consultation on changes and affords staff opportunities to influence suggestions.
■ Workers are informed of the likely consequences of any changes to their positions. Employees receive training, if necessary, to support any changes to their jobs;
■ Workers are informed of changing timelines; and
■ During transitions, employees have access to relevant support.
References
https://www.who.int/news-room/fact-sheets/detail/mental-health-at-work
5.5 VIOLENCE AT WORK
What is Violence?
The Health and Safety Executive defines workplace violence as follows: (a) “any occurrence in which a person is abused, intimidated, or assaulted in work-related circumstances.”
(b) Verbal abuse and threats are the most frequent forms of violence. Physical attacks are rather uncommon.
Who is at risk?
Those whose jobs compel them to interact with the public may be vulnerable to violence. Most vulnerable are those who engage in:
■ giving a service
■ Caring
■ Education
■ Cash transactions
■ delivery/collection
■ controlling
■ representing authority
What the law requires
There are five key health and safety laws that pertain to workplace violence.
They include:
■ The Health and Safety at Work etc. Act 1974 (HSW Act)
Employers are required by law to guarantee their employees’ health, safety, and wellbeing at work, so far as is reasonably practicable.
■ The Management of Health and Safety at Work Regulations 1999
Businesses are required to evaluate the hazards to their employees and make arrangements for their health and safety by:
– planning;
– Organization;
– Control;
– Monitoring and review.
The risks should, when applicable, include the requirement to protect employees against exposure to violence that is reasonably foreseeable.
■ The Reporting of Injuries, Diseases and Dangerous Occurrences
Regulations 1995 (RIDDOR)
Employers must notify their enforcement authority in the event of a workplace accident resulting in the death of an employee, a serious injury, or incapacity for normal work for at least three consecutive days. This includes any nonconsensual act of physical assault against an employee.
■ Safety Representatives and Safety Committees Regulations 1977 (a) and
The Health and Safety (Consultation with Employees) Regulations 1996 (b)
Companies must provide employees with timely information and consultation regarding their health and safety. Employee representatives, either nominated by recognized trade unions or elected by their co-workers (a) or elected under (b) may communicate with their employer about concerns endangering the health and safety of persons they represent.
Effective management of violence at Work
A straightforward four stage management process is set out below-
Stage 1 Finding out if you have a problem
Stage 2 deciding what action to take
Stage 3 Take action
Stage 4 Check what you have done
Stage 1 Finding out if you have a problem
The first step of risk assessment is hazard identification. You may believe that workplace violence is not a problem or that incidences are uncommon. But, your staff may have a quite different perspective.
Ask your staff – Do this informally through managers, supervisors, and safety advocates, or utilize a brief survey to see if your staff ever feel endangered. Inform them of the results of your survey to demonstrate that you identify the issue.
Keep detailed records It is advisable to document instances, such as verbal abuse and threats. You may find it beneficial to jot down the following details:
■ An account of what happened;
■ details of the victim(s), the assailant(s) and any witnesses;
■ the outcome, including working time lost to both the individual(s) affected and
to the organization as a whole;
■ the details of the location of the incident.
Classify all incidents – Use headings such as location, time, event type, potential severity, parties involved, and likely causes. It is essential that you study each event report to see whether a more severe outcome could have occurred. Here is an example of a simple classification for determining the severity of incidents:
■ fatal injury;
■ major injury;
■ injury or emotional shock requiring first aid, out-patient treatment, counselling,
absence from work (record number of days);
■ feeling of being at risk or distressed.
Try to predict what might happen – Do not limit your evaluation to occurrences that have already impacted your personnel. There may be a pattern of violence associated with particular job conditions. Trade and professional organizations and labor unions may have important information regarding this. Local, national, and technical press articles may help inform you of pertinent happenings and prospective issue areas.
Stage 2 deciding what action to take
Having discovered that violence could be a concern for your staff, you must determine the appropriate course of action. Continue the risk assessment by completing the steps below, which will assist you in determining the necessary course of action.
Decide who might be harmed, and how
Identify which employees are at risk – Those that interact with the public face-to-face are typically the most susceptible. Whenever possible, identify potentially violent individuals in advance in order to limit the dangers associated with them.
Evaluate the risk
Examine the current safety precautions; are they sufficient, or should more be done? Keep in mind that violence is typically caused by a mix of causes. Variables which you can affect include:
■ the level of training and information provided;
■ the environment;
■ the design of the job.
Consider the way these factors work together to influence the risk of violence.
Training and information
Teach your employees to recognize the early warning signs of hostility so that they can either avoid or deal with it. Ensure that they completely comprehend any security measures you’ve implemented.
Give personnel with any information they may require to identify clients with a history of violence or to predict factors that may increase the likelihood of violence.
The environment
Offer improved seating, dcor, and lighting in public waiting areas, as well as more frequent updates on delays.
Consider the following physical security measures:
■ Video cameras or alarm systems;
■ coded security locks on doors to keep the public out of staff areas;
■ wider counters and raised floors on the staff side of the counter to give staff more protection.
The design of the job
Use checks, credit cards, or tokens instead of cash to reduce the appeal of robbery.
Increase the frequency of your bank visits and vary your route to lessen the chance of robbery.
Verify the credentials of clients and the location and logistics of any off-site meetings.
Arrange for employees to be escorted by a coworker if they must meet a potential aggressor at their residence or in a remote area.
Make preparations for remote personnel to stay in touch with their home office.
Sustain staffing levels to prevent a lone worker situation from arising.
Record your findings
Document the major findings of your evaluation. The document should serve as a working document for both management and staff.
Review and revise your assessment
Periodically verify that your evaluation accurately reflects your current work environment. Be willing to add additional measures or modify existing measures when they are ineffective. This is especially crucial when a job is changed. If a violent occurrence occurs, reassess your assessment and make any necessary adjustments.
Stage 3 Take action
Your policy for addressing violence could be included in your health and safety policy statement, so that all employees are aware of it. This will aid your employees in cooperating with you, adhering to protocols, and reporting additional events.
Stage 4 Check what you have done
Regularly evaluate the effectiveness of your arrangements, consulting with employees or their representatives. Consider establishing joint management and safety committees for this purpose. Maintain records of incidents and review them frequently; they will demonstrate your progress and whether the situation is evolving. If your measures are effective, maintain them.
If violence remains a problem, consider a different approach. Return to Stages 1 and 2 and discover other preventive measures that may be effective.
References-
https://www.hse.gov.uk/pubns/indg69.pdf
5.6 SUBSTANCE ABUSE AT WORK
Businesses are required by law to protect the health, safety, and welfare of their employees. Knowing the indicators of drug and alcohol misuse (or abuse) will enable you to manage health and safety risks in the workplace, create a strategy to address drug-related issues, and provide support for your staff.
What the issues are and what to look out for
Abuse is not equivalent to dependence. The use of illegal narcotics and the abuse of alcohol, pharmaceuticals, and chemicals such as solvents constitutes drug and alcohol abuse.
Consider the following indicators of substance or alcohol abuse:
How to Manage Substance Abuse Issues?
Consult your employees
Employees or their representatives must be consulted on health and safety problems. Consultation entails not only providing information to employees but also listening to and considering their feedback.
You might ask your employees about their knowledge of the consequences of drugs and alcohol on health and safety, as well as the restrictions or guidelines governing drug and alcohol usage in your workplace.
Look at safety-critical work
Consider the nature of your profession and any safety-critical aspects where drug or alcohol abuse could have severe consequences.
for example:
Develop a policy
An agreed-upon policy on drug/alcohol abuse can help all organizations. You might include a policy on drugs and alcohol in your overall health and safety policy.
An effective policy should strive to aid and support an employee who discloses a drug or alcohol issue, rather than result in termination.
But it should also indicate when you will take disciplinary or other action, such as immediately reporting drug possession or distribution to the authorities.
When personnel in safety-sensitive positions seek treatment for alcohol or drug abuse, it may be necessary to temporarily transfer them to a different position.
You could incorporate screening and testing for drugs and alcohol in your policy if you elect to do so.
Screening and testing for drugs and alcohol
Some employers have incorporated testing into their drug and alcohol policies. If you choose to do the same, you should carefully consider the purpose of screening and what you will do with the information it provides.
There may be a reason for screening, especially in specific occupations (for example employees who make safety-critical decisions like drivers, pilots and some machinery operators). In these positions, the usage of drugs or alcohol could have catastrophic consequences for the individual, his or her coworkers, the general public, and the environment.
Bear in mind that:
Support employees with a drug or alcohol problem
After assessing the risk and establishing a policy for drug or alcohol misuse (or abuse) in the workplace, ensure that your employees are aware of the policy and the support you provide.
Training and awareness
Provide a description of the drug and alcohol misuse policy in the onboarding process for all new workers to enhance awareness.
You could also brief managers and supervisors so they are clear about:
Support for employees
Workers with a drug or alcohol problem may seek assistance at work if they are assured that their issues will be handled discretely and in confidence. Consider your own legal position if proof or information indicates that an employee’s drug abuse has resulted in workplace violations.
Alcohol and drug addiction are recognized medical conditions. A person who is abusing drugs or alcohol has the same rights to privacy and assistance as someone with any other medical or psychiatric issue.
Urge them to seek assistance from their primary care physician or a specialized drug or alcohol agency, and recommend them to the occupational health department of your organization (if you have one).
Consider granting someone time off to obtain expert assistance. Frequently, the cost of hiring and training a new employee exceeds the cost of time off.
Consider whether your workplace treats drug and alcohol abuse as a disciplinary matter or a health concern. An employment tribunal may determine that you have terminated someone unfairly if you fire them for drug or alcohol abuse without attempting to help them.
But, if their typical job is safety-sensitive, you may need to temporarily transfer them to a different position.
Health advice and information
Even without occupational health services, you can still support the health and welfare of your employees. You can ensure that employees have access to information on where they can go for guidance and assistance if they are concerned about drug or alcohol abuse.
The law
Under the Health and Safety at Work etc. Act, you have a general obligation to ensure the health, safety, and welfare of your employees so far as is practically practicable. Also, employees must take reasonable care of themselves and anyone whose health may be harmed by their work. There is up-to-date information on regulations pertaining to drug and alcohol abuse, such as the Misuse of Drugs Act of 1971 and the Road Traffic Act of 1988. Frank also possesses useful legal knowledge.
References